Sedation Dentistry for Children: Safe, Stress-Free Dental Visits for Your Child

Reviewed By Dr. Dennis Rollins, DDO |
July 2025 • 6 min Read
Reviewed By Dr. Dennis Rollins, DDO | July 2025 • 6 min Read
Sedation is a safe and common technique used by pediatric dentists for extensive treatments, and when a child has anxiety, fear, or special needs. It helps children feel relaxed, comfortable, and less aware of the procedure. Side effects are almost always mild, and the child typically feels completely normal again after a day resting at home.
Your dentist can help you determine if sedation is right for your child and which type would be best for them.
Common Pediatric Sedation Types at a Glance
| Sedation Type | Effects | Onset and Recovery |
|---|---|---|
| Nitrous oxide (laughing gas): Delivered through a small mask over the nose. Used for routine procedures and for mild anxiety. | The child feels floaty and relaxed but stays awake. | Works within minutes and wears off quickly. |
| Oral sedation: Used for longer procedures and for moderate anxiety. | The child feels calm and sleepy and may doze off. | Works in 20–45 minutes. Most children are sleepy for one to several hours after. |
| IV sedation: Used for extensive treatments and with children with severe anxiety or a strong gag reflex. | The child will feel sleepy or fall asleep. | Works within 2-5 minutes. The child will feel groggy for several hours after. |
| General anesthesia: Used in surgical settings and for children who are very young, have severe anxiety, and/or special needs. | The child will be fully asleep. | Works within a few minutes. Recovery can take several hours. |
| Effects | Onset and Recovery |
|---|---|
| Nitrous oxide (laughing gas): Delivered through a small mask over the nose. Used for routine procedures and for mild anxiety. | |
| The child feels floaty and relaxed but stays awake. | Works within minutes and wears off quickly. |
| Oral sedation: Used for longer procedures and for moderate anxiety. | |
| The child feels calm and sleepy and may doze off. | Works in 20–45 minutes. Most children are sleepy for one to several hours after. |
| IV sedation: Used for extensive treatments and with children with severe anxiety or a strong gag reflex. | |
| The child will feel sleepy or fall asleep. | Works within 2-5 minutes. The child will feel groggy for several hours after. |
| General anesthesia: Used in surgical settings and for children who are very young, have severe anxiety, and/or special needs. | |
| The child will be fully asleep. | Works within a few minutes. Recovery can take several hours. |
What to Expect and Do Before, During, and After a Procedure
Before the Procedure
Typically, you’ll be asked not to let your child eat or drink for several hours before the procedure. This reduces the risk of nausea and vomiting while they’re under sedation. Make plans for the rest of the day, since your child typically should not return to school or active play directly after undergoing sedation.
On the day, dress your child in loose, comfortable clothes, and bring an item your child finds comforting, whether it’s a blanket, a stuffed animal, or a small toy. Explain the procedure to them in simple terms. Assure them that they’ll be safe the entire time, and that the dentist and their team will take good care of them.
Before treatment begins, the dentist or anesthesiologist will review your child’s medical history, allergies, medications, and any past experiences with anesthesia or sedation.
During the Procedure
If laughing gas or mild oral sedation is being used, parents are typically allowed to stay nearby to help reassure the child. If the treatment plan involves IV sedation or general anesthesia, parents are usually asked to stay in the waiting room. This is because the dental team needs a sterile, distraction-free environment to monitor the child’s breathing and heart rate.
Feel free to ask about these safety procedures ahead of time, so that you and your child can be prepared.
The dental team will closely monitor your child throughout the procedure. With laughing gas, the dental team carefully watches your child’s breathing, skin color, and responsiveness throughout the visit. Oxygen is always delivered along with the gas, and electronic monitors can be used if your child has special medical needs or the dentist prefers added safety checks.
With oral sedation, the team keeps a close eye on your child’s comfort and alertness. A pulse oximeter is often used to measure oxygen levels and heart rate, and the dental team will check breathing and blood pressure at regular intervals.
During IV sedation, the monitoring is more advanced. Your child’s heart rate, breathing, oxygen level, and blood pressure are continuously tracked by electronic monitors, and often a capnography device is used to measure carbon dioxide levels.
With general anesthesia, an anesthesiologist or anesthesia team continuously tracks heart rate, blood pressure, oxygen, breathing rate, and carbon dioxide levels from start to finish.
After the Procedure
When treatment is complete, the team will monitor your child until they’re awake, stable, and alert enough to go home. With laughing gas, recovery is almost immediate. With oral sedation, IV sedation, or general anesthesia, they may feel sleepy or groggy for several hours.
When you get them home, encourage them to rest for the remainder of the day.
Once your child is fully alert, you can offer them clear fluids and soft foods, so long as they’re not feeling nauseous. Follow any post-operative instructions for pain management, diet, and oral hygiene.
After sedation, it’s normal for children to feel a little sleepy, dizzy, or unsteady for a few hours. Some may be irritable, emotional, mildly nauseous, or take a longer nap than usual. These are common responses, and children almost always feel back to normal the next day.
When to Call the Dentist
If any of the following symptoms occur, it’s a good idea to call your dentist. While they don’t necessarily mean something serious is wrong, they can signal that your child needs to be checked to make sure everything is okay.
- Persistent vomiting may mean your child’s stomach hasn’t fully settled from the medication, or that they swallowed some blood during dental treatment.
- Trouble breathing or severe coughing could indicate irritation from the procedure, mucus in the airway, or (very rarely) a reaction to the sedation medicine.
- A high fever might suggest an infection, dehydration, or inflammation from the procedure.
- Prolonged drowsiness can happen if your child’s body is taking longer to clear the sedation medication. Most of the time this resolves on its own, but your dentist may want to evaluate oxygen levels and recovery progress.
- Unusual behavior (confusion, agitation, or not acting like themselves) is typically temporary, but persistent changes should be checked out.
These symptoms are uncommon and shouldn’t cause alarm. Calling the dentist right away ensures they can quickly rule out anything serious and help your child recover comfortably and safely.
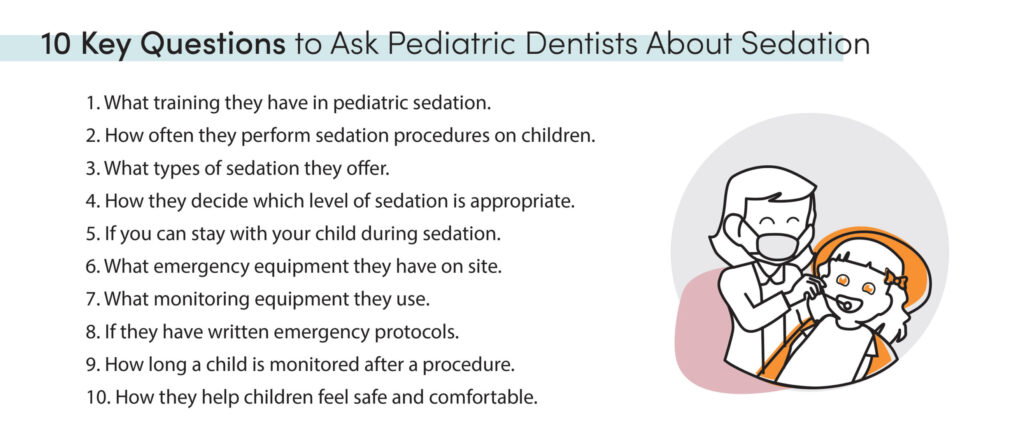
Questions to Ask When Choosing a Pediatric Dentist
Because it’s so important to be informed and feel confident when choosing your child’s dentist, you should feel free to ask as many questions as you like. You can call and get your answers from the front office team or request a short call with the dentist.
Below are questions worth asking.
Credentials and Experience
Ask:
- If they’re a board-certified pediatric dentist.
- What training they have in pediatric sedation.
- How often they perform sedation procedures on children.
- If they’re certified in Pediatric Advanced Life Support (PALS) or Basic Life Support (BLS).
Sedation and Bedside Manner
Ask:
- What types of sedation they offer.
- How they decide which level of sedation is appropriate.
- How they calculate medication doses for children.
- If they’ll provide a written consent form explaining the risks, benefits, and alternatives to sedation.
- What post-sedation instructions they’ll provide.
- If you can stay with your child during and after sedation.
- How they help children feel comfortable and reduce anxiety.
Emergency and Safety
Ask:
- What emergency equipment they have on site.
- If they have written emergency protocols and if they conduct regular emergency drills.
- Where the nearest hospital is, and what their plan is if a child needs to be transferred.
- What monitoring equipment they use during sedation.
- Who monitors vital signs during the procedure?
- How they ensure a child’s airway remains open and safe.
- How long a child is monitored after a procedure.
- How they follow up after a procedure.
For help finding a pediatric dentist in your area, click here or call us at (888) 597-3896.
Managing Dental Anxiety for You and Your Child
It’s normal for parents and children to feel anxious about a dental procedure, and children often look to their parent to know how nervous or relaxed they should feel. To help keep yourself and your child calm, consider these methods.
- Try to schedule the procedure first thing in the morning, so that neither of you spends the day anticipating it.
- Without rushing, show up a little early to the appointment, giving your child time to get used to the environment.
- Take slow breaths, smile, and speak softly. Your confidence helps your child feel safe.
- Tell your child what’s going to happen in simple, positive language.
- Talk about other things, like their favorite activities, your family pet, and something fun you’ll do together after the appointment.
- Let the dental team take the lead. They’re trained in child-friendly communication and comfort techniques.
- Keep in mind that these procedures are routine and that you’ve chosen your child’s dentist carefully.
Need Help Finding a Pediatric Dentist?
Related Information

Broken Tooth Repair Cost: From Bonding to Crowns
If you’ve chipped or cracked a tooth, you’re likely dealing with two problems at once: physical discomfort and financial panic. You’re not just wondering “How bad is this?”, you’re wondering “How much will this cost me?” This guide gives you clear, realistic price ranges, explains what affects the cost, and shows you how acting quickly can save you hundreds, or even thousands, of dollars.

How Much Is a Dentist Visit Without Insurance? Exact Costs Explained
Below, you’ll find a breakdown of typical out-of-pocket costs for common dental procedures, along with the reasons behind these costs. Keep in mind that these costs can vary significantly based on your location, the dentist’s experience, the materials used, and the complexity of the procedure.
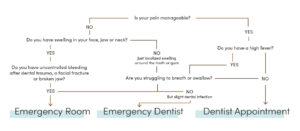
Should You Go to the ER for Tooth Pain? A Quick Guide
Whether you should go to the ER for tooth pain depends on the severity of your pain and what other symptoms you’re experiencing. Read on for help deciding how to find relief.
